Study: Ivermectin Promotes Peripheral Nerve Regeneration during Wound Healing
I have stayed out of the Ivermectin discussion until now.
I am unsure if anyone has commented on this study, but here it is.
Most people are commenting on the spike protein and cancer aspect.
The study:
https://pubs.acs.org/doi/10.1021/acsomega.8b01451
I’ve heard from several people who had modRNA injections and suffered injury, who have burning pain, who may or may not have a diagnosis of an autoimmune demyelination, small fiber neuropathy, etc. that ivermectin is helping them.
This study looks at the impact of ivermectin on wound healing and the positive impacts peripheral nerve healing.
Study Abstract:
”Peripheral nerves have the capacity to regenerate due to the presence of neuroprotective glia of the peripheral nervous system, Schwann cells. Upon peripheral nerve injury, Schwann cells create a permissive microenvironment for neuronal regrowth by taking up cytotoxic glutamate and secreting neurotrophic signaling molecules. Impaired peripheral nerve repair is often caused by a defective Schwann cell response after injury, and there is a critical need to develop new strategies to enhance nerve regeneration, especially in organisms with restricted regenerative potential, such as humans. One approach is to explore mechanisms in lower organisms, in which nerve repair is much more efficient. A recent study demonstrated that the antiparasitic drug, ivermectin, caused hyperinnervation of primordial eye tissue in Xenopus laevis tadpoles. Our study aimed to examine the role of ivermectin in mammalian nerve repair. We performed in vitro assays utilizing human induced neural stem cells (hiNSCs) in co-culture with human dermal fibroblasts (hDFs) and found that ivermectin-treated hDFs promote hiNSC proliferation and migration. We also characterized the effects of ivermectin on hDFs and found that ivermectin causes hDFs to uptake extracellular glutamate, secrete glial cell-derived neurotrophic factor, develop an elongated bipolar morphology, and express glial fibrillary acidic protein. Finally, in a corresponding in vivo model, we found that localized ivermectin treatment in a dermal wound site induced the upregulation of both glial and neuronal markers upon healing. Taken together, we demonstrate that ivermectin promotes peripheral nerve regeneration by inducing fibroblasts to adopt a glia-like phenotype.”
The study looked at both in vitro and in vivo using ivermectin on mice and wound healing.
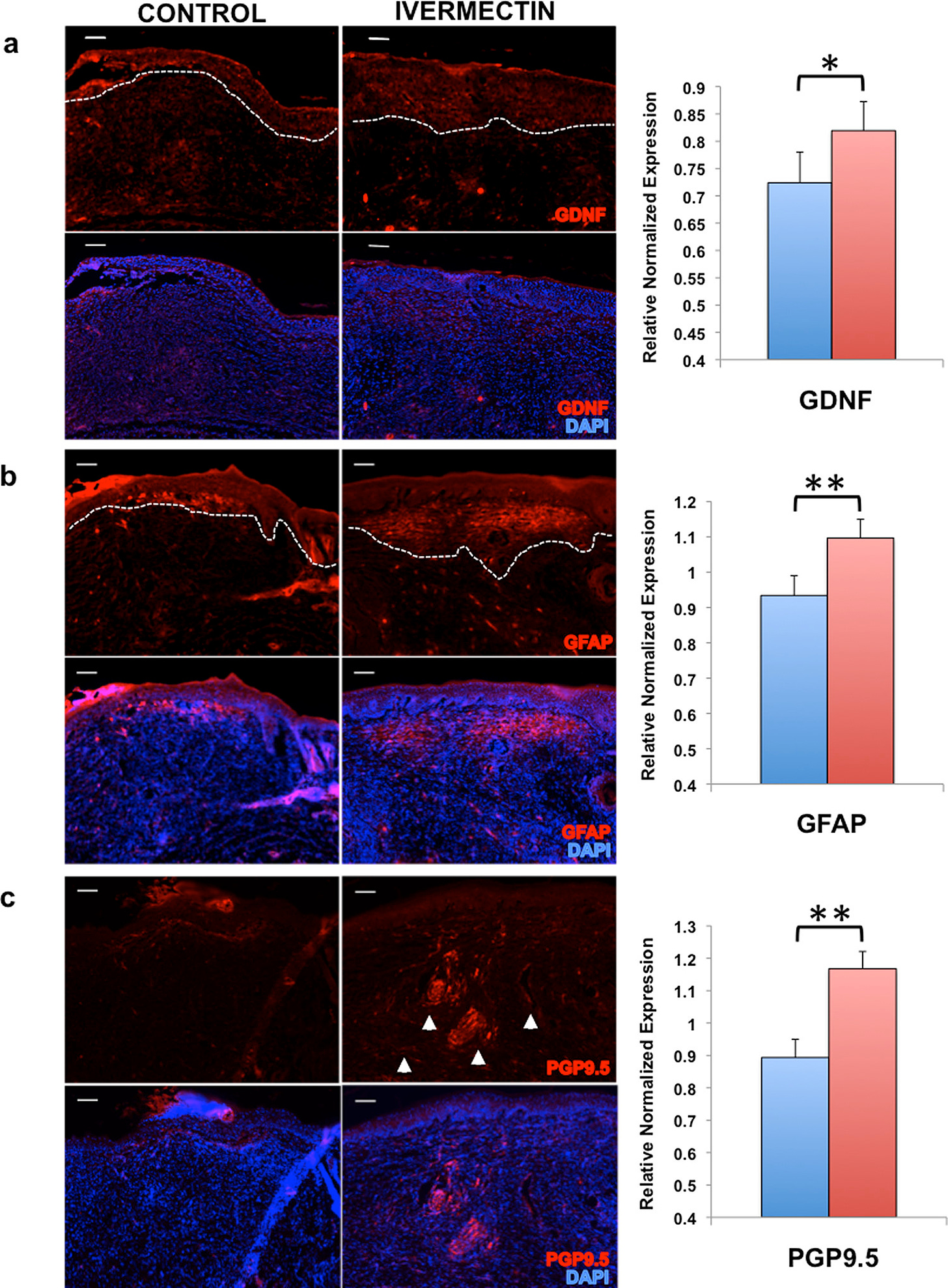
The in vitro experiments demonstrated ivermectin converts dermal fibroblasts into a glial-like phenotype, supporting neuronal growth. The scientists then used a dermal wound healing model in mice to show nerve repair with ivermectin. Ivermectin-treated wounds improved healing compared to controls. Additionally, the researchers looked at the effects of ivermectin’s action on various ion channels and receptors, its potential for enhancing peripheral nerve repair, and its application in clinical settings.
Previous studies in Xenopus laevis tadpoles demonstrated that ivermectin treatment of non-neuronal stromal tissue promotes nerve growth from adjacent neuronal tissue. This study aimed to determine whether these effects are replicable in mammalian systems, specifically assessing ivermectin's impact on human-induced neural stem cells (hiNSCs) and its efficacy in a murine wound healing model.
Results
In Vitro Studies
In co-culture experiments, hiNSCs exposed to ivermectin-treated fibroblasts showed increased proliferation and migration.
Ivermectin treatment induced fibroblasts to adopt a glial-like phenotype, characterized by enhanced uptake of extracellular glutamate, expression of neurotrophic factor GDNF, and features typical of Schwann cells. These transformed cells provided a supportive environment for nerve growth.
In Vivo Studies
A dermal wound healing model in BALB/c mice was used to assess ivermectin’s in vivo effects.
Two full-thickness skin biopsies were performed, with one wound treated with ivermectin-loaded collagen gels and the other with a control (DMSO).
Ivermectin-treated wounds demonstrated significantly smaller sizes compared to controls at days 8–9 and 11–12, indicating enhanced healing.
The researchers found ivermectin’s role in nerve regeneration by promoting a glial-like phenotype in fibroblasts and supporting neuronal growth. The drug's effects align with recent studies emphasizing the importance of peripheral glia in tissue regeneration.
A little more science:
Neuronal Migration Assay
The researchers created a transwell system where hDFs were seeded in the bottom chamber and treated with either DMSO (control) or 1 μM ivermectin. These cells were repeatedly washed to remove any residual drug.
Predifferentiated human neurons, labeled with DiD and expressing β III tubulin (Tuj1) (a pan-neuronal marker), were seeded onto the membrane in the top chamber. This ensured that the assay was measuring neuronal migration and not cell proliferation.
The transwell systems were cultured overnight in low serum media to minimize the potential for any remaining proliferation.
Results
Ivermectin-treated hDFs caused a significant increase in neuronal migration compared to the control group. This suggested that the treated fibroblasts were influencing the surrounding environment in a way that promoted neuron movement, which is essential for nerve repair.
Investigating the Role of Glutamate
The researchers hypothesized that one of the reasons for the increase in neuronal migration could be related to the removal of cytotoxic glutamate from the extracellular environment by ivermectin-treated hDFs.
To test this, they treated hDFs with varying concentrations of ivermectin and measured the extracellular glutamate levels in the cell culture media.
Interestingly, they found that ivermectin-treated fibroblasts significantly reduced the concentration of extracellular glutamate in a dose-dependent manner, suggesting that these cells might uptake glutamate, which is released by neurons following injury.
To investigate this, hDFs were treated with either a vehicle or 1 μM ivermectin for 4 days and subjected to qRT-PCR to assess the expression of various neurotrophic factors.
There was no significant change in the expression of brain-derived neurotrophic factor (BDNF) or nerve growth factor (NGF). However, ivermectin-treated hDFs showed a dramatic upregulation of glial cell line-derived neurotrophic factor (GDNF), which is typically expressed by astrocytes and Schwann cells.
Protein Level Confirmation and Secretion
Immunostaining showed that GDNF expression increased significantly with exposure to ivermectin concentrations ≥1 μM.
To confirm that GDNF was also being secreted, an ELISA was performed on conditioned media from hDFs treated with various concentrations of ivermectin. The results showed that at concentrations ≥2.5 μM, ivermectin caused significant GDNF secretion.
However, concentrations ≥5 μM were found to be cytotoxic in vitro.
Role of GDNF in Neuronal Migration
To understand if GDNF played a role in the effects of ivermectin-treated hDFs on hiNSC migration, the migration assay was repeated (as in Figure 2) using a GDNF-blocking antibody.
The antibody reduced the migration-promoting effects of ivermectin-treated hDFs, indicating that GDNF plays a significant role in the neuronal migration observed.
Glial-like Transformation of hDFs
The study also explored whether ivermectin-treated hDFs adopted characteristics similar to glial cells.
After treatment with increasing concentrations of ivermectin for up to 8 days, hDFs showed upregulation of several genes related to Schwann cell biology, including Sox10, S100B, myelin basic protein, GAP43, and NCAM1.
Upregulation of GFAP and Morphological Changes
hDFs treated with 1 μM ivermectin exhibited significantly higher expression of glial fibrillary acidic protein (GFAP) at both 4 and 8 days, suggesting a transition toward a glial phenotype.
Immunostaining also revealed morphological changes in the treated hDFs, which became thin and elongated, similar to Schwann cells.
The researchers found ivermectin might have a small impact on wound closure, but ivermectin’s potential for clinical applications in nerve repair needs more research. It is already FDA-approved for parasitic infections, and it could be repurposed for peripheral nerve repair. Ivermectin's action on various ion channels and receptors, coupled with its effects on glial cells and GDNF secretion, shows potential for other applications of ivermectin.
This is really something that could help people, and it looks like for burning pain with autoimmune nerve pain and damage, this could be what is helping people with long covid and modRNA covid injection injury.




Really interesting news you got there.
I have been treating my neuropathy with just heat lamps, but this might convince me to try a more comprehensive red light therapy.
.https://blissandblisters.substack.com/p/red-light-district